Hepatobiliopancreatic Surgery
Hepatobiliary and Pancreatic Surgery – A Center of Excellence in Advanced Minimally Invasive Techniques
Our center is internationally recognized for its expertise in hepatobiliary and pancreatic surgery, with a strong focus on minimally invasive approaches. Since the early 2000s, our surgical team—led by our Professor and Head of Department—has been at the forefront of innovation in this field. At a time when liver and pancreatic procedures were almost exclusively performed via open surgery, he was among the first in the world to develop and adopt minimally invasive techniques for these complex interventions.
As a true pioneer, he played a key role in establishing the international guidelines for minimally invasive liver and pancreatic surgery. He actively contributed to consensus conferences, helped validate best practices, and published numerous scientific articles that shaped the evolution of the discipline worldwide.
Today, our team continues this legacy of innovation. We perform advanced laparoscopic and robotic procedures for a wide range of benign and malignant hepatobiliary and pancreatic conditions, offering patients the benefits of minimally invasive surgery: reduced postoperative pain, shorter hospital stays, faster recovery, and optimal oncological outcomes.
With decades of experience, a multidisciplinary team, and access to cutting-edge technology, our center represents a national and international reference point for safe, effective, and evidence-based hepatobiliary and pancreatic surgery.
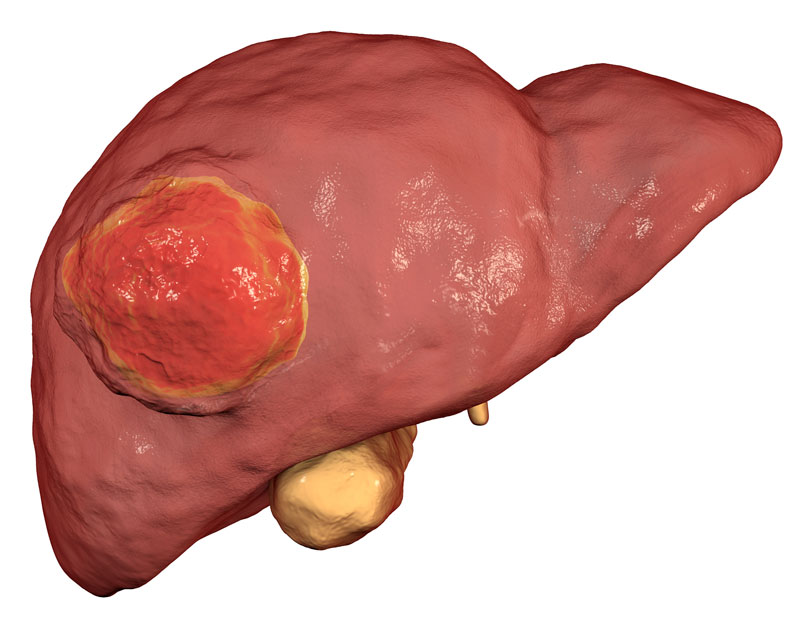
1. Liver Cancer
Hepatocellular Carcinoma (HCC) is the most common primary liver tumor. It originates from hepatocytes, primarily due to chronic liver disease or cirrhosis.
Causes
The main causes of hepatocellular carcinoma are hepatitis B or C and cirrhosis. Its occurrence in a healthy liver is much rarer. For this reason, individuals with these conditions are advised to undergo regular blood tests to help prevent the potential development of this cancer.
Symptoms
Early stages of hepatocellular carcinoma are typically asymptomatic. Patients most often present with symptoms typical of advanced cirrhosis:
- Bleeding from esophageal varices
- Jaundice
- Enlarged hemorrhoids
- Loss of appetite
- Abdominal distension (swelling of the abdomen)
- Pain in the upper abdomen radiating to the shoulder blade
Diagnosis
Early diagnosis is crucial, as hepatocellular carcinoma is more treatable in its initial stages. Specific blood tests are necessary at first. These are systematically followed by imaging studies: ultrasound, CT scan, or MRI. A biopsy may sometimes be required.
Treatment
Treatment of hepatocellular carcinoma depends on the tumor's progression and the presence of underlying chronic liver disease (cirrhosis, hepatitis). If liver function is preserved, surgical resection of the affected area is possible.
Surgery: Our department specializes in surgical management of both benign and malignant liver lesions, based on a thorough and individualized assessment.
- A complete evaluation is carried out and discussed in a multidisciplinary team meeting.
- Main treatment options: surgery or radiological techniques (e.g., embolization)
Surgical approaches: laparoscopic (a field in which our professor is internationally recognized as an expert) or controlled laparotomy
- Back to eating the next day
- Hospital stay approximately one week
- Intensive care if needed
Risks:
- Pulmonary complications
- Bleeding
- Bile leaks
If liver function is impaired due to cirrhosis, non-surgical strategies are preferred:
- Radiofrequency ablation
- Microwave ablation
- Radiotherapy
- Endovascular radiotherapy
...and other case-specific options.
Liver transplantation may be considered for selected patients.
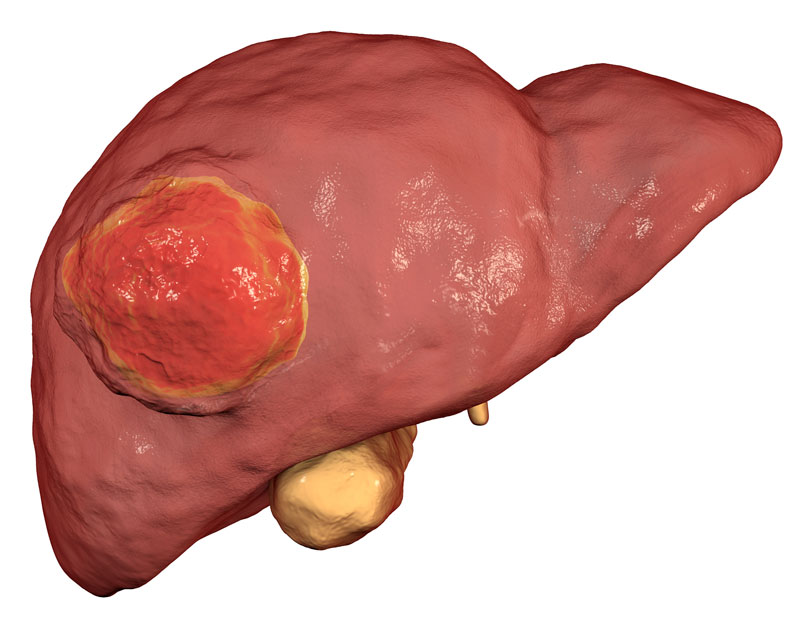
Liver Metastases
Liver metastases, also known as secondary liver tumors, originate from cancer cells outside the liver. These cells typically migrate from other organs (most commonly the colon or rectum) to the liver.
Symptoms
Liver metastases often remain asymptomatic for a long time. Main symptoms may include:
- Pain in the upper abdomen, sometimes radiating to the shoulder
- Fatigue
- Weight loss
- Loss of appetite
- Nausea or vomiting
- Jaundice
- Cachexia (wasting syndrome)
Diagnosis
Imaging is essential for accurately characterizing liver metastases:
- Ultrasound
- Magnetic Resonance Imaging (MRI)
- CT scan
- Positron Emission Tomography (PET scan)
These exams determine the location, size, and number of lesions. A biopsy may be indicated in some cases. For patients with known primary cancers (especially colorectal, gastric, esophageal, pancreatic, renal, lung, breast, or skin), regular liver monitoring is recommended.
Treatment
Management is case-dependent:
- Surgery: Hepatic resection offers the best outcomes, particularly for colorectal metastases
- Chemotherapy: Can reduce the size of metastases to facilitate surgery
- Innovative therapies:
o Targeted therapies (biologic drugs)
o Immunotherapy
o Radioembolization
o Stereotactic radiotherapy
These approaches now enable long-term control in many patients.
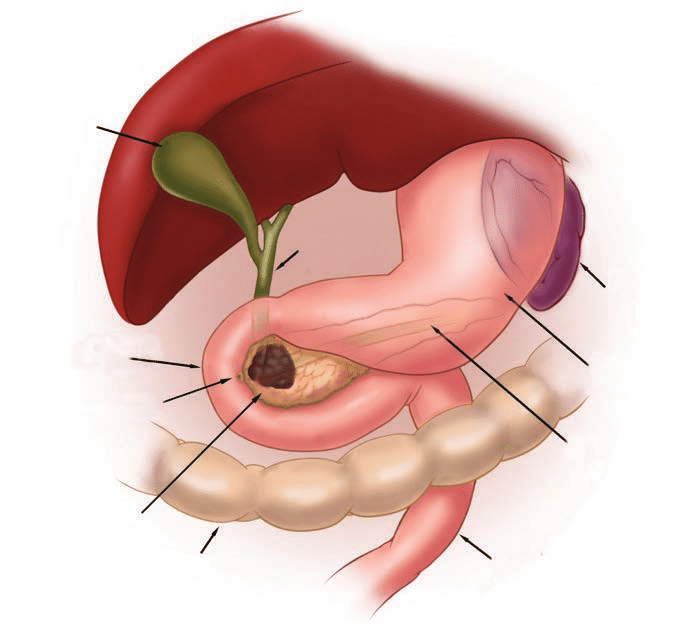
2. Pancreatic Cancer (Adenocarcinoma)
The most common type of pancreatic cancer is adenocarcinoma. It typically develops in the head of the pancreas and originates from the ducts that carry digestive enzymes.
Highly aggressive and prevalent, it affects over 10,000 people annually, mainly between ages 60 and 80, with an equal gender distribution.
Due to its rapid spread to the lungs and liver and the difficulty of early diagnosis, it is one of the most challenging cancers to treat.
Causes
Pancreatic cancer results from the uncontrolled growth of genetically altered cells. While the origin of these alterations is often unknown, several risk factors are identified:
- Overweight and obesity
- Chronic pancreatitis
- Smoking (risk nearly tripled among smokers)
- Age (> 60 years)
- Family history of cancers linked to hereditary genetic mutations (e.g., breast, colon)
- Diet high in animal proteins and fats
Symptoms
Early diagnosis is difficult due to the absence of specific symptoms. Signs usually appear only after bile duct obstruction or disease spread:
- Loss of appetite and weight
- General weakness
- Nausea and vomiting
- Upper abdominal pain radiating to the back
- Jaundice
- Diabetes
Diagnosis
A specialist confirms the diagnosis using:
- CT scan
- MRI
- Endoscopic ultrasound
Tumor markers in the blood can support diagnosis. In case of jaundice, additional exams are needed.
Endoscopic ultrasound (via gastroscope) allows for biopsies when needed (suspicious lesions or neoadjuvant chemotherapy).
Treatment
Structured patient care pathway :
- Specialized consultation
- Comprehensive staging work-up
- Collegial decision at a multidisciplinary consultation meeting (RCP)
Our surgical excellence: Laparoscopy and/or controlled laparotomy
- Proximal and distal tumors: minimally invasive laparoscopy (4–5 trocars) and/or controlled laparotomy
Treatment strategy depends on imaging-assessed stage:
- Resectable tumor: Complete removal with healthy margins
- Locally advanced tumor: Involvement of visceral arteries → initial chemotherapy to reduce vascular invasion, followed by surgical re-evaluation
- Metastatic cancer: Surgery is contraindicated except in rare cases (young patients in good condition who respond well to chemotherapy, decision validated by the tumor board)
Post-operative follow-up:
- Adapted diet (D1 to D4 depending on complexity)
- Hospital stay: 3-12 days (+ intensive care if necessary)
- Close monitoring at 3 weeks, then every 3-6 months
Other Pancreatic Tumors
Cystic Pancreatic Tumors
These heterogeneous lesions are often discovered incidentally during abdominal ultrasounds. They require morphological characterization by MRI.
- Benign lesions Radiological monitoring
- Borderline/malignant lesions Surgical resection
Neuroendocrine Tumors (NETs)
These tumors arise from cells that secrete digestive hormones (glucagon, insulin, gastrin):
- 70% non-secreting : Asymptomatic hormonal.
Diagnosis :
- Hypervascularity on contrast-enhanced CT
- Nuclear medicine imaging (PET scan with Dotatoc®, Gallium PET)
Treatment :
- Functioning tumors: Systematic surgical removal
- Non-functioning tumors:
- < 2 cm → Surveillance
- 2 cm → Surgery
Prognosis : Depends on size, lymph node involvement, metastases, and Ki-67 proliferation index.
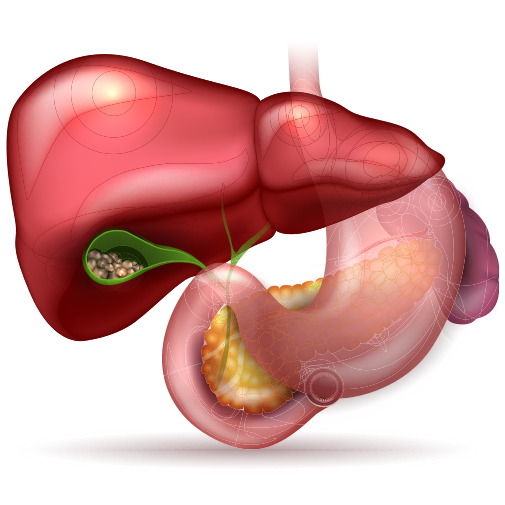
3. Gallstones (Cholelithiasis)
Gallstones are solid particles that form in the gallbladder and may sometimes migrate into the bile ducts. This is a common condition, affecting approximately 25% of individuals over the age of 50. It is more frequent in women and individuals who are obese or have certain medical conditions. Gallstones can be made of cholesterol (about 80%) or bile pigments (20%).
Symptoms
Many people with gallstones experience no symptoms. When symptoms do occur, they can include:
- Pain: Upper abdominal pain, typically after eating fatty foods, lasting less than six hours.
- Nausea, vomiting, pain radiating to right shoulder
- If a gallstone blocks the bile duct, it can lead to complications like jaundice, cholangitis (infection of the bile ducts), or pancreatitis.
Treatment
- Cholecystectomy:
The standard treatment for symptomatic gallstones is the removal of the gallbladder. This is usually performed through laparoscopy (minimally invasive surgery with small incisions). - Advanced techniques: Our team performs micro-laparoscopy (2-3 mm incisions).
- Stones in the Bile Duct:
If a stone moves into the bile duct, it may be treated with an endoscopic procedure to widen the bile duct opening (sphincterotomy).

Risks
- Bleeding: Usually controlled during the laparoscopic procedure.
- Bile Duct Injury: This can occur in cases of significant infection or unusual anatomy. Our team is highly experienced in managing these rare complications.
Post-operative Care
- After surgery, patients are typically seen for a follow-up appointment one week later (if treated as an outpatient) or one month later (if hospitalized).
- Most people recover quickly and do not require long-term monitoring.
Subsribe To Our Newsletter
Stay in touch with us to get latest news.
Address
Hôpital Antoine-Béclère 157 rue de la Porte de Trivaux, 92140 Clamart, France
Call Us
Reception: 6:45 - 17:00, Monday to Friday. Tel: +33 1 45 37 43 43 39 | +33 1 45 37 43 43 48
Call Us
Medical secretariat: 8:30 - 17:00, Monday to Friday. Tel: +33 1 45 37 43 43 39 | +33 1 45 37 43 43 48
Email Us
Cécile.huber@aphp.fr
Ibrahim.dagher@aphp.fr
